Medical coding system expanded
Published 10:27 am Friday, May 24, 2013
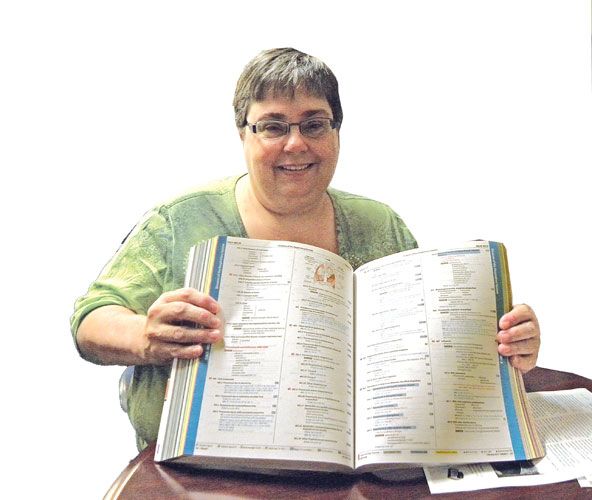
- Susan Nason displays the new medical coding book that coders will learn from. Nason is in charge of the Health Information Department at Grande Ronde Hospital where she will help train personnel in the federally mandated ICD-10 medical coding system.
Old system is being upgraded nationwide to one that has 115,000 alpha-numeric codes, each 5 to 7 digits long
LA GRANDE – Medical coders throughout the United States are under a federally mandated deadline to learn and utilize an entirely new set of medical codes by Oct. 1, 2014.
The current International Classification of Diseases Ninth Revision or ICD-9 was developed by the World Health Organization, and it has been in use by coders since 1979. This system with its 24,500 codes seems simplistic now compared to the highly specific ICD-10 system, which has 115,000 alpha-numeric codes, each five to seven digits long.
The codes are used for a variety of purposes: for epidemiology studies and research to determine the best treatment and to trend; to develop new service specialists for the patient population; for reimbursement of services by Medicare, Medicaid and other insurance providers; and to publish select coding data for consumers over the Internet.
For hospitals, making the transition to an expansive coding system will require re-training, and to facilitate this, Grande Ronde Hospital has hired Kforce Healthcare of Portland. This consulting and training firm has already trained a core group of five or six hospital personnel in the ICD-10 system. But it’s just the beginning as 16 medical coders be impacted by the changeover, as well as the billing department, registration, human resources along with staff physicians and nurses. With a deadline looming, all will need to prepare to achieve ICD-10 readiness.
The ICD-10 upgrade will cause a ripple effect that will require other necessary changes within the hospital, including a software upgrade, revisions to hospital forms and restructuring of the billing process.
Susan Nason, RHIA, is the manager of the Health Information Management department at Grande Ronde Hospital and a certified ICD-10 trainer. She is poised to help the hospital staff learn the new system.
“Medicare estimates that the education needed for each coder is greater than 50 hours,” Nason said. “It is imperative for physicians and nursing professionals to be proficient in the bolstered ICD-10 requirements of documentation in order to fully utilize and take advantage of the robust data this new coding system can provide. Each physician will need approximately 15 hours of education to expand their documentation practices.”
Presently, medical coders spend an average of 20 minutes coding a single inpatient visit. With the ICD-10 system, coders may be spending 50 to 70 percent more time on each patient visit, building a medical code that fully describes the patient’s visit to the physician.
For example, a patient presenting with a malunion of a fracture (fracture not healing properly) will be assigned a medical code that reflects which bone is involved, the location of the bone or what part of the bone and if it includes a joint. The new code will also indicate if this is the patient’s first time seeing the specialist. The former ICD-9 system does not have that kind of flexibility.
The ICD-10 is capable of describing weird accidents or circumstances that cause injuries. Some patients may have received injuries from being struck by a baseball bat (code W2111XA) or perhaps injured while boarding a plane (V971XXA). On the other hand, a person may have been bitten by an alligator while scuba diving (W5803XA, Y9315).
“It codes for diseases, signs, symptoms, abnormal findings, complaints, social circumstances and external causes of injury or disease,” Nason said. “It also codes for noncompliance, under-dosing or refusal to accept treatment due to religious or spiritual reasons. The code Z53.1 would indicate that the patient refused a blood transfusion due to religious beliefs or philosophy.”
Medical codes provide a way for health organizations to examine and publish trends such as in the World Health Organization’s mortality and morbidity booklet. The robust data held in this coding system can be sorted by disease type, gender, age and many other criteria. An analysis of the sorted data can be used to substantiate the need for a local hospital to hire a particular disease specialist for the community.
Statistical data is given to the state registry, including accidents and specific diagnoses.
“Also, private and public sectors use codes to determine ratings for both hospital and physicians at websites such as HealthGrades and HospitalCompare,” she said.
“In the last three decades, coding has also been used as a billing tool,” Nason said. “Codes must be submitted on every bill that comes out of a hospital or any other health care setting. Medicare uses these codes to determine payments for services.”
Learning a new and expansive system like ICD-10 means hospitals and clinics will more than likely experience a fall in reimbursements from Medicare, Medicaid and insurance providers because of mistakes in coding or insufficient information on the patient’s EHR.
“We can’t just go to a doctor and ask him about the patient’s case,” said Nason. “We have to go by what is written on the patient’s record.”
To gradually ease into the new numbers, Nason said the coders will be doing “dual coding” using both the ICD-9 and ICD-10 systems starting in June 2014. This gives the coders several months to learn the new system while still maintaining quality output with the present system of coding.
Nason is optimistic that Grande Ronde Hospital is ready for the transition.
“We are totally committed to making this as good as we can get it,” Nason said.








